What You Need to Know When Building a Telemedicine App
Contents
Contents
Telehealth and telemedicine are the fastest-growing niches in the healthcare IT industry in the post-pandemic times, as we explored earlier, powered by technological breakthroughs and rising popularity among patients and medical workers.
Although “telemedicine” and “telehealth” are often used as synonyms, telemedicine focuses on remote medical services— diagnosis and treatment provided by primary care specialists. Telehealth broadly encompasses mobile apps, healthcare education resources, remote patient monitoring, and other technology to improve people’s health and well-being. In today’s article, we’ll look at how to develop a telemedicine app and what you’ll need to know before getting started.
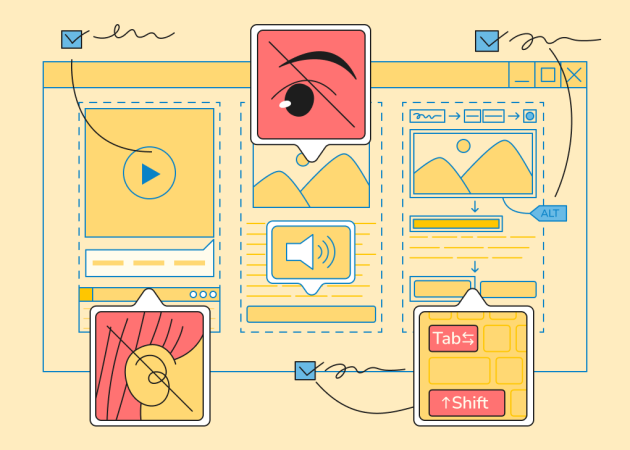
How do telemedicine apps work?
Telemedicine allows clinicians to treat patients whenever needed, regardless of location, using a computer or smartphone equipped with a camera, microphone, and custom software. A typical online consultation workflow may include the following:
- To receive a consultation, a patient logs into the system (a new or existing account) and chooses related symptoms, specialists, and services;
- After finding a doctor, a patient books an appointment (video call) using a built-in calendar.
- The doctor and patient receive a visit confirmation, then hold a scheduled visit;
- Doctor asks for medical history during the online consultation, communicates about the symptoms, and prescribes treatment and lab tests.
- After the call, the patient carries out online payment using a built-in payment gateway and receives receipts with prescribed meds and doctor’s recommendations.
Challenges of telemedicine
Interoperability
The nature of health data poses a paradox: it is difficult to share because it is sensitive and requires a high level of privacy and security, yet its inability to be accessed when needed has the potential to do substantial harm. A lack of interoperability and “understating” among various healthcare IT systems can result in additional barriers to care provision, higher expenses, and administrative pressure.
At its finest, developing interoperable solutions relies on a holistic approach: combining the right technology with strong core capabilities to improve the patients’ access to their data and facilitate secure and seamless data exchange at all levels.
Compliance with healthcare laws and regulations
Any healthcare provider who handles Protected Health Information (PHI) in the United States must follow the Health Insurance Portability and Accountability Act (HIPAA). Examples of PHI are imaging like MRI and CT scans, lab test results, and physician’s notes.
Information gathered or processed in the EU is subject to GDPR (General Data Protection Regulation), even if it relates to a non-EU citizen. As a result, if a US-based organization handles sensitive data of EU citizens or residents, it must be GDPR-compliant. The same principle applies to European firms operating in the EU and US markets.
Your chosen software team — regardless of whether it is in-house or provided by a development partner — must understand and comply with the regulations governing your field to focus on data protection.
Language barriers
While improving healthcare for some population categories, digital health can throw more hurdles for others. For example, in the United States, 25.6 million people with limited English proficiency face many social, economic, and cultural challenges exacerbated by healthcare systems and technologies designed with English speakers in mind. So it’s vital to ensure that outreach is packaged in a way that all patients can access care, especially those with chronic conditions, regardless of the language they speak.
Tech stack needed to develop a telehealth app
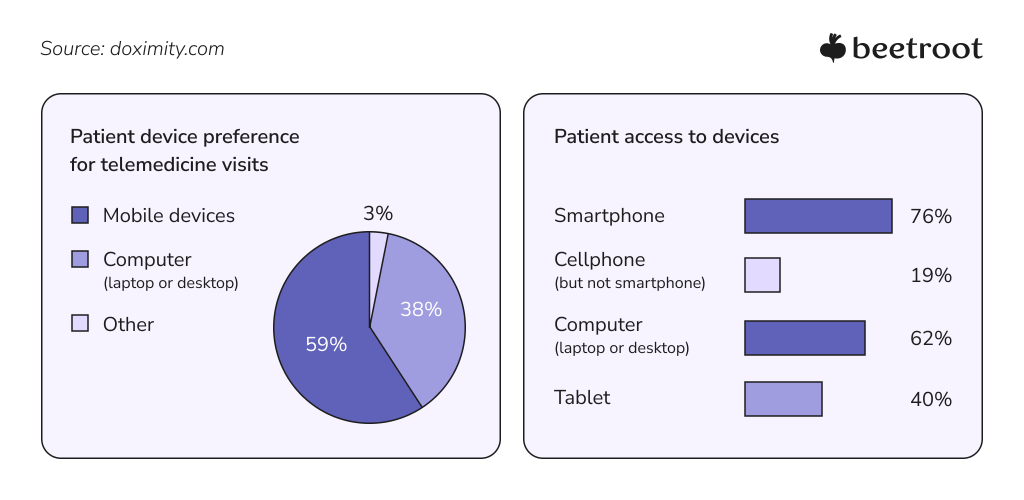
The choice of the technology stack will heavily depend on your business vision and goals, the type of platform (web, mobile, or other), developer availability, inherent security, development speed, and ultimate cost. Regarding platforms, Doximity’s recent report finds that 59% of patients prefer mobile devices for telemedicine. Mobile phones, in particular, are the most accessible device type across all categories of the population in the US.
While there’s undoubtedly no one-size-fits-all solution here, you can find some of the most popular instruments that telehealth software engineers choose to work with below.
- Front-End/UI: JS frameworks such as Angular or React;
- Backend: Python/Ruby/Java;
- iOS: Swift;
- Android: Kotlin/Java;
- Cross-Platform: React Native/Flutter;
- Data storage: MySQL, Hbase, MongoDB, Postgres, Cassandra;
- Cloud: Amazon Web Services (AWS), Google Cloud;
- Micro-services: Node.js, Express.
A lot depends on the team that will execute your development project. So if you need advice regarding the skills to look for when hiring developers, take advantage of our newest guide or contact us directly to talk with an expert consultant.
Discovery stage in telemedicine app development
Discovery is generally the stage of gathering project information and finalizing the app specifications. It is one of the most challenging phases in telemedicine app development because your requirements are the foundation for all subsequent steps. Some of the key points you’ll have to work through during discovery include:
Validating your idea
First, identify specific problems your telemedicine app solves, study your target audience by interviewing people who match your desired buyer persona profile, find out the strengths and weaknesses of your competitors and determine your own. The information you collect from researching the market and your target audience will help you craft your value proposition and turn it into a unique selling proposition (USP) by adding specificity.
Finding a reliable technology partner
Telehealth solutions require specific domain expertise, so it might be reasonable to use the services of a software development company with a proven track record in HealthIT. But what are the aspects you’d have to consider when choosing a potential development partner?
- Their relevant experience
In addition to mining customer reviews on Clutch and other databases, check the social media of the company’s executives and key employees. Survey your shortlisted candidates on their developer standards, the technology spectrum they work with, and cross-domain competence. The nature of their experience should be explicit early in the project discovery process.
- Approach towards communication
Assessing the possible communication risks, including the time zone and cultural differences, is crucial when hiring an offshore development team. You may also directly inquire about the agency’s communication framework and available solutions to mitigate possible discrepancies.
- Suitable collaboration model
When building a telemedicine app from scratch, the most popular engagement models are outsourcing and outstaffing. Outsourcing cooperation suggests delegating the end-to-end development process to your tech partner. It is the optimal setup for non-tech-savvy entrepreneurs who need to quickly bring their idea to market. The outstaffing model, aka Team Extension or Dedicated Team, is a way of upscaling your in-house team with hand-picked talent recruited specifically for your project roles. This model gives you complete control over the development process while cutting hiring timelines for the open positions in your in-house team.
- Flexibility to match the scope of your project
When selecting a technology partner, telehealth companies frequently overlook the agency’s ability to expand or downscale a development team in response to project course changes. So it is essential to clarify the project’s requirements, your expected timeline and deliverables, and the remote team’s flexibility from the beginning.
- Handling proprietary and sensitive data
During your research, identify if the software developed by the contractors you shortlisted has licensing or usage fees. To avoid major issues later on, you must document your exclusive rights to the project and include an intellectual property (IP) clause in the contract. It is also critical to thoroughly investigate your potential partner’s information security and data protection approach.
Cost evaluation of telemedicine app development
How much does it cost to develop a telemedicine app? The key factors affecting the cost of telemedicine app development are:
- Development team’s location
Just as much as in any other software development domain, the cost of hiring developers to build your health application will vary from country to country. Here are some hints on the best places to find healthcare developers.
- Team size
A primary team for developing a telemedicine app from the ground up typically consists of 8-10 people. The roles involved are business analyst, product owner, project manager, UI/UX designer, iOS/Android developer, backend developer, and QA engineer.
- Application platform
Hint: the cost of developing a native telehealth app for Android is higher than for iOS since the QA specialists should test Android apps on different devices.
- App size
The total number of features, such as doctor and patient databases, appointment scheduling, secure video calling, and chatbot, to name a few, determine the app’s size.
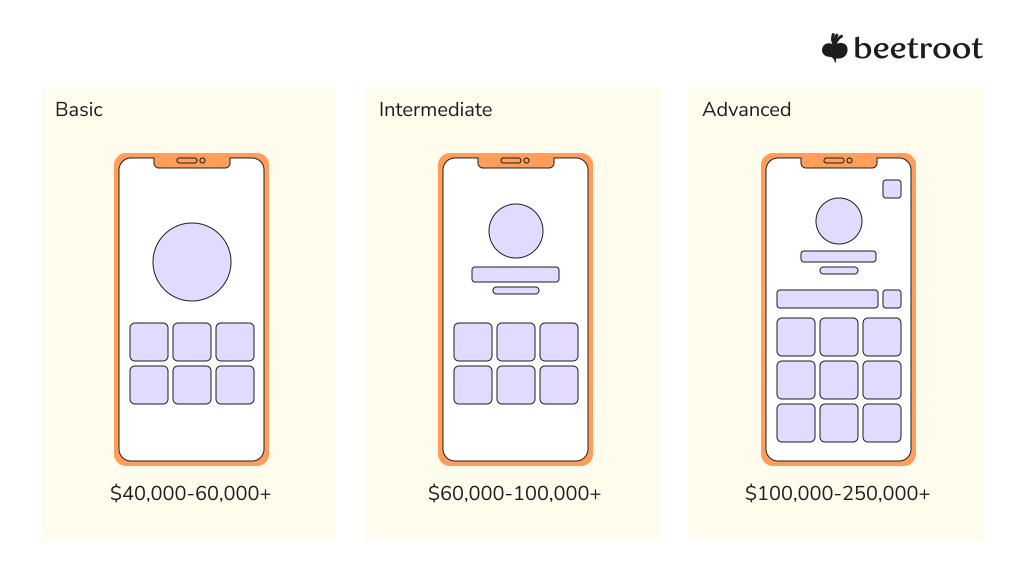
Based on the above factors, you can expect a ballpark estimate of your telemedicine app development cost to lie within these ranges:
Developing an MVP
A Minimum Viable Product (MVP) is the “raw” version of a new product — enough to test the concept and quickly establish a foothold in the market. It focuses on the core functionality that provides value to your target users and enables your team to collect validated feedback during the first iteration.
“Before developing an MVP, make sure it will have demand in the market. The first essential steps include defining a problem to solve with your app and creating buyer persona(s). After that, we suggest starting agile and developing a Mocked MVP, which mocks data storage and demonstrates UI for the end-user confirming or denying your hypotheses.”
Dmytro Barbashov, CTO at Beetroot
Although there is no universal formula for a healthcare app, let’s briefly review some of the functional essentials you can include in your MVP.
Personal profiles
Besides storing credentials, patients should set up personal preferences, choose a location and enable data synchronization with the available medical records (EHRs, EMRs) because physicians need to view the clinical information before and during consultations.
Doctors’ profiles should provide their qualifications, work experience, certification, ratings, working hours, and access to the required internal information.
Secure video conferencing
Visuals should be transmitted in the highest possible quality, even at low latency, since doctors rely on video cues to identify signs of illness and diagnose.
It would be best to optimize your real-time connection, for example, by utilizing the RTMP and WebRTC streaming protocols. And, of course, GDPR/HIPAA compliance is a must for your in-app video chat.
Built-in text messaging
Some matters are too minor to discuss through a video call or book an individual appointment. So a peer-to-peer chat is an excellent option for patients, and their physicians to exchange text messages before, during, and after a call, provide written instructions, attach multimedia files, and clarify treatment details.
Backend database
One of the many requirements for a telemedicine application is a secure repository for patient health records, imaging, prescriptions, and relevant medical data. Backend integration with a reliable database such as MongoDB or Redis stores this information and makes it accessible to the app users while keeping the data exchange between them secure and synchronized. However, with HIPAA compliance and other regulations in mind, choosing an optimal backend infrastructure is challenging and needs a thorough analysis of all product requirements.
Appointment scheduling
Patients need to view their scheduled appointments, check their physicians’ availability, reschedule consultations and receive notifications once the doctor confirms the visit. Allow doctors to plan and manage their calendars, cancel and reschedule appointments, and notify patients accordingly.

Healthcare app architecture development
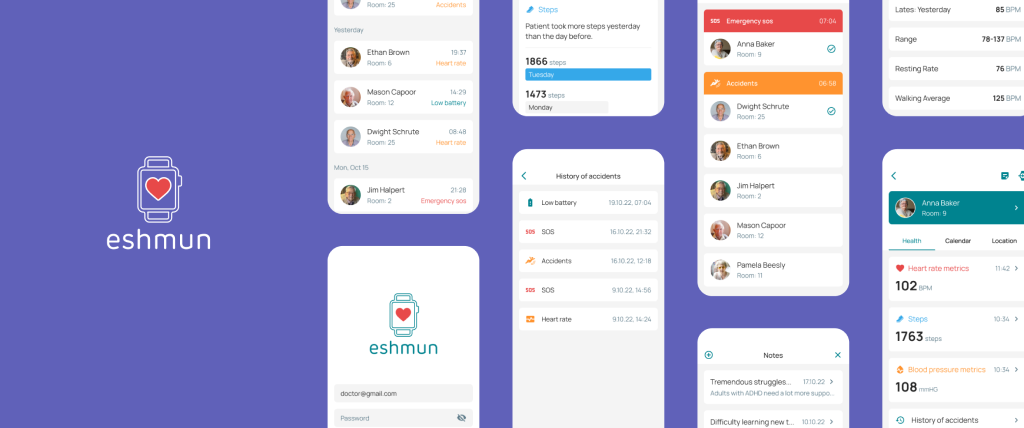
After deciding on the features and technology to include in your product, the next step is to design the architecture. It serves as the glue that holds all of your technological decisions together. Let’s use Beetroot’s in-house R&D project, the Eshmun telenursing app, as an example of multi-level app architecture.
- Clients
Eshmun serves three types of clients: patients, caregivers, and platform administrators (one for each user group). Currently, it provides a dashboard for caregivers (nurses, family members, and other care providers) to overview a patient’s health and treatment data, accessible via a web portal and mobile app.
- Communication Components
The Eshmun app uses proprietary devices to enable real-time communication (voice messaging, live chat, alerts) between patients and caregivers. Here, compliance with designated regulative standards, such as HIPAA, GDPR, or PIPEDA, is mandatory.
- API & Management
The databases for the app clients are linked together using an API and microservices system. Finally, the management layer executes the app’s business logic to collect, process, store, and route data to users and other software. Task examples include routing, authentication, notification, and pub/sub.
- Storage & Infrastructure Services
The app uses cloud-based services. Google JSP, in particular, hosts the API and business logic layer, stores user and business data, and manages IT infrastructure. It, in turn, contains functional modules such as raw data storage, MVC, and background operation completion.
To summarize, data collected by the Eshmun app flows between clients and the API & Management layer hosted on Google JSP.
Closing words
The global healthcare industry is shifting toward a more proactive model, which telehealth applications greatly facilitate. Telemedicine solutions have changed how patients access healthcare, receive treatment, and interact with their doctors.
We don’t just ‘write code’ or provide software solutions here at Beetroot. We guide your HealthTech product to success by augmenting teams and building engineering capacity for any healthcare development area, ranging from custom CRMs, cloud-based EHR development, and integrations to lab automation and LMS software. So let’s talk and see how we can facilitate your project.
Subscribe to blog updates
Get the best new articles in your inbox. Get the lastest content first.
Recent articles from our magazine
Contact Us
Find out how we can help extend your tech team for sustainable growth.